Ear infections are more than just a painful nuisance – they can also affect how well we hear. Understanding the link between ear infections and hearing loss is important for people of all ages.
Ear infections are very common (especially in children) and often the number one reason parents take their child to the doctor.
Along with discomfort and fussiness, an ear infection can cause sounds to become muffled or harder to hear.
The good news is that in most cases this hearing difficulty is temporary, and knowing what to do can help protect long-term hearing.
In this post, we’ll explore what ear infections are, how they impact hearing, who is most at risk, and how to prevent and treat them.
Key Takeaways
- Ear infections, especially middle ear infections, are a common cause of temporary hearing loss, particularly in children.
- There are three types of ear infections: outer, middle, and inner, each with different causes and symptoms.
- Most ear infection-related hearing loss is temporary and hearing typically returns to normal after the infection clears up.
- Repeated or severe ear infections can lead to more significant or even permanent hearing loss in rare cases.
- Preventive measures like vaccinations, good hygiene, and avoiding tobacco/smoking can reduce the risk of ear infections.
What is an Ear Infection?
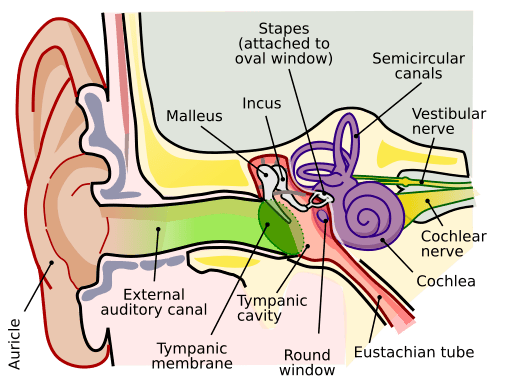
The ear has three main parts – the outer ear, middle ear, and inner ear – and all three can get infected [1].
When doctors talk about an “ear infection,” they usually mean a middle ear infection (the space right behind the eardrum), but infections can also occur in the ear canal or deep inside the inner ear.
Here are the three types of ear infections and their typical causes and symptoms:
- Outer ear infection (otitis externa) – This affects the ear canal, the tube that carries sound from the outside to your eardrum. A common example is “swimmer’s ear,” often caused by water remaining in the ear or injury from placing objects like cotton swabs in the canal. It leads to a red, swollen ear canal that hurts to touch, sometimes with discharge, and can cause temporary hearing loss because the swollen canal blocks sound [2].
- Middle ear infection (otitis media) – This happens behind the eardrum, in the air-filled space with the tiny hearing bones. It often starts after a cold or sore throat when the eustachian tube (which drains fluid from the middle ear) gets blocked [3] Fluid builds up and bacteria or viruses grow in that fluid, causing pain and often fever. The eardrum may look red or bulging. Middle ear infections are most common in children, and they frequently cause muffled hearing while fluid or swelling is present.
- Inner ear infection (otitis interna or labyrinthitis) – This is an infection of the inner ear, where the hearing organ (cochlea) and balance organs (vestibular system) are located. Inner ear infections are less common but can happen, often due to a virus. They can cause sensorineural hearing loss (affecting the nerves of hearing) and often balance problems like dizziness or vertigo. People with an inner ear infection might feel extreme spinning sensations and nausea in addition to hearing loss. Inner ear infections usually don’t produce the ear pain that outer or middle ear infections do, but they can have a more serious impact on hearing and balance.
Many people notice some hearing difficulty during an ear infection. In fact, hearing loss is one of the most common side effects of a middle ear infection [4].
When the outer or middle ear is infected, sound vibrations cannot travel as well to the inner ear – imagine listening with ear plugs in. In a middle ear infection, fluid trapped behind the eardrum makes it harder for the eardrum and tiny bones to move, causing what’s known as a conductive hearing loss.
On average, a middle ear infection with fluid can cause about a 24 decibel reduction in hearing – roughly equivalent to the sound being as quiet as a whisper [5].
People might say things sound muffled or faint. The good news is that this type of hearing loss is usually temporary. As the infection clears and fluid drains, hearing typically returns to normal.
However, severe or repeated ear infections can lead to longstanding hearing changes. Ongoing infections or chronic fluid in the middle ear can damage the eardrum or the tiny ossicle bones, leading to more significant hearing loss [6].
In rare cases, a spread of infection to the inner ear can cause permanent damage to the hearing nerve. Inner ear involvement (for example, in a severe middle ear infection or labyrinthitis) may result in permanent hearing loss if the delicate cochlea is harmed.
Fortunately, such serious complications are not common – most ear infections do not lead to permanent hearing problems [7].
The key is to treat ear infections properly and monitor hearing, so any lingering issues can be addressed early.
Who is at Risk for Ear Infections?
Anyone can get an ear infection, but some groups are more prone than others:
- Young children – Infants and children under age 3 get ear infections most often [8]. Their eustachian tubes (the drainage tubes between the middle ear and throat) are shorter and more horizontal than in adults, which makes it easier for fluid and germs to get trapped [9]. Young children also have developing immune systems and tend to catch more colds (especially if they attend daycare), which can lead to ear infections [10]. It’s estimated that five out of six children will have at least one middle ear infection by their third birthday [11].
- Children with a predisposition – Kids who spend time in group daycare or preschool are exposed to more colds and bugs, raising their risk of ear infections [12]. Family history plays a role too – if parents or siblings had frequent ear infections, a child might be more susceptible [13]. Babies who are bottle-fed (especially while lying flat) may have a higher risk than breastfed babies, partly because breastfeeding can help boost immunity and the swallowing motion helps clear the ears. Additionally, children with allergies, asthma, or cleft palate, or those around secondhand smoke, tend to get ear infections more easily [14].
- Adults – Although ear infections are often thought of as a childhood issue, adults can absolutely get them. Adult ear infections may happen after an upper respiratory infection or due to chronic sinus issues or allergies that block the eustachian tubes. Adults with weakened immune systems or chronic conditions are also at risk. Exposure to cigarette smoke or air pollution increases the risk for both children and adults, as it can irritate and inflame the ear’s airways [15]. Swimmers (of any age) have a higher chance of outer ear infections if water stays in the ear canal. Even wearing earbuds or hearing aids without proper cleaning can sometimes lead to outer ear infections by introducing bacteria. The bottom line: children are more likely to get ear infections than adults [16], but people of any age should be aware of the risk factors, especially if they have frequent colds or other contributing factors.
Long-Term Consequences: When Does Temporary Hearing Loss Become Permanent?
Most of the time, the muffled hearing that comes with an ear infection improves once the infection is treated or clears up.
Fluid behind the eardrum will gradually drain away or be absorbed, and the eardrum and bones return to normal movement.
So in typical cases, any hearing loss during an infection is temporary and hearing returns to baseline within a short time [17].
It’s still important to follow up, especially for young children – doctors may check that fluid is gone and possibly test hearing to ensure everything is back to normal.
Problems arise when ear infections become frequent or long-lasting (chronic). Repeated infections can eventually cause damage.
For example, ongoing inflammation can scar the eardrum or cause it to thicken, reducing its flexibility. In some cases, the pressure from chronic fluid can erode parts of the middle ear or cause a small hole in the eardrum that doesn’t heal.
Conditions like a cholesteatoma (an abnormal skin growth in the middle ear from chronic infection) can develop and permanently affect hearing if not removed.
According to medical experts, complications of long-term ear infections can include permanent injury to the ear structures and even partial or complete deafness in the affected ear [18, 19].
Fortunately, this outcome is rare and usually happens only when infections go untreated for a long time or keep happening over and over.
Consistent medical care – and surgical interventions like ear tube placement when needed – greatly reduce the chance of permanent hearing loss. Remember that most ear infections do not cause lasting hearing problems [20].
Being aware of the signs of complications (like hearing that doesn’t come back after an infection) and seeking timely care can prevent minor, temporary issues from becoming permanent.
Prevention and Treatment: Protecting Your Ears and Hearing
Knowing how to prevent ear infections, and how to treat them if they occur, can spare you a lot of pain and protect your hearing.
Here are some prevention tips and treatment approaches to keep ear infections under control:
Prevention Tips
- Stay up to date on vaccines – Keeping immunizations current (especially the pneumococcal vaccine and annual flu shots) can prevent infections that often lead to ear infections [21]. For example, the pneumococcal vaccine helps protect against a common bacteria that causes middle ear infections [22].
- Practice good hygiene – Wash hands frequently and avoid close contact with people who have colds whenever possible. This can reduce the spread of the viruses and bacteria that trigger ear infections [23].
- Breastfeed infants if possible – Breastfeeding for at least the first 6–12 months can lower a baby’s risk of ear infections [24]. Breast milk contains antibodies that help fight infections, and the swallowing motion helps keep the eustachian tubes clear. If bottle-feeding, try to hold the baby at an incline rather than flat on their back to help prevent milk from entering the middle ear via the eustachian tube.
- Avoid smoke and allergens – Do not smoke, and keep children away from secondhand smoke [24]. Cigarette smoke exposure irritates the lining of the ear and eustachian tubes, making infections more likely [25]. Also manage environmental allergies with proper medication, since allergies can cause ear fluid build-up.
- Keep ears dry and clean – For those prone to outer ear infections, it helps to dry your ears thoroughly after swimming or bathing [26]. You can gently towel-dry or use ear drops (ask your doctor for recommendations) to prevent “swimmer’s ear.” Avoid inserting foreign objects (cotton swabs, fingers, etc.) into the ear canal, as these can damage the skin and introduce germs.
- Flu season care – During cold and flu season, take extra care: treat nasal congestion promptly (with saline nasal sprays or as advised by your doctor) to help keep eustachian tubes open. Teaching children to blow their nose gently and one nostril at a time can also help clear the ears.
Treatment and Management
- Watchful waiting – Often, ear infections (especially mild middle ear infections) will get better on their own as the body fights off the infection [27]. If symptoms are not too severe, doctors might suggest a “wait and see” approach for 2-3 days while managing pain at home
[28]. Many viral ear infections or mild bacterial cases will clear without antibiotics. - Medication – If the infection is caused by bacteria or isn’t improving on its own, a course of antibiotic ear drops (for outer ear infections) or oral antibiotics (for middle ear infections) may be prescribed [29. 30]. It’s important to use the medicine exactly as directed and finish the full course, even if symptoms improve sooner. For pain and fever, age-appropriate doses of acetaminophen or ibuprofen can help keep a child (or adult) comfortable. Never give aspirin to children due to the risk of Reye’s syndrome.
- Ear tubes for chronic cases – For children (or adults) who experience frequent ear infections or fluid buildup that just won’t go away, doctors may recommend tiny ventilating tubes in the eardrums. These ear tubes (placed during a brief outpatient surgery) allow fluid to drain and air to circulate in the middle ear, preventing future infections and helping restore hearing [31]. Ear tubes typically stay in place for about a year and often fall out on their own as the eardrum heals [32]. This procedure can greatly improve quality of life for kids who have fluid in their ears month after month. If enlarged adenoids are contributing to blocked eustachian tubes, an ENT specialist might also suggest removing the adenoids to improve ear health.
- Inner ear infection care – If someone has an inner ear infection or vestibular neuritis, treatment is usually supportive: rest, hydration, and sometimes medications like steroids or antivirals depending on the cause. Balance therapy exercises might be needed if dizziness is severe. Quick medical attention is important for inner ear issues to reduce the risk of permanent effects.
- Protect hearing during infections – While your ear is healing, avoid loud noises or pressure changes (like flying on an airplane) if you can, since the ear is more sensitive. It’s okay to ask for a follow-up hearing test after a tough infection. In fact, children with long-lasting fluid may get a hearing exam to ensure they’re not experiencing ongoing hearing loss [33]. This can guide further treatment. Taking ear infections seriously and attending follow-up appointments is part of protecting your long-term hearing.
When to Seek Medical Help
Ear infections can usually be managed at home for a few days, but certain warning signs mean you should see a healthcare provider promptly:
- High fever or severe symptoms – If you or your child has a fever higher than 102.2°F (39°C)
[34], or if the ear pain is excruciating, seek medical care. Severe headache, stiff neck, or swelling around the ear are also red flags that need urgent evaluation. - Ear discharge – Pus, blood, or fluid draining from the ear is a sign of a possible eardrum rupture or a serious infection [35]. While eardrum tears often heal on their own, you’ll need a doctor to examine the ear and possibly prescribe antibiotics to prevent further complications [36].
- Worsening or prolonged symptoms – If symptoms last more than 2-3 days without improvement or are getting worse [37] (for example, the pain is increasing or new symptoms appear), it’s time to see a doctor. The infection might not be clearing on its own and could need medication.
- Noticeable hearing loss or balance problems – Temporary muffled hearing is common, but if you notice you cannot hear well at all from the affected ear, or if you have new dizziness, let a healthcare provider know. Significant hearing loss should always be checked, and it’s especially important for children – untreated ear issues can impact speech development [38].
- Very young infants – For babies under 3 months old, any fever (100.4°F / 38°C or higher) should be taken seriously [40]. Young infants can get sick quickly, so don’t wait if you suspect even a possible ear infection or if your little one is inconsolable. It’s always okay to call the pediatrician if you are concerned.
In general, trust your instincts – if something feels very wrong, or pain is severe, seek medical help. It’s better to have an ear checked and find out it’s a minor issue than to miss a developing complication.
Final Thoughts
Ear infections can be scary, especially when they affect your or your child’s hearing. But remember, you’re not alone and these infections are highly treatable. Most ear infections clear up without any long-term effects on hearing [40].
By knowing the signs and taking simple preventive steps, you can reduce the chances of infections and catch them early when they do happen.
Always feel empowered to ask doctors questions about your ear health – whether it’s understanding the treatment plan or requesting a hearing test to ease your worries.
In a compassionate light, an ear infection is usually a temporary hurdle, not a life-long roadblock. With proper care (and a bit of patience during the healing process), hearing typically returns to normal and the pain subsides.
If you or your family members are prone to ear infections, keep up with the strategies that work (like staying up to date on vaccines and avoiding smoke) and have a plan with your healthcare provider.
And if you’re ever unsure, don’t hesitate to seek a medical opinion – early attention can prevent complications and give you peace of mind.
Understanding the connection between ear infections and hearing loss means you can act quickly and sensibly. You’ve armed yourself with knowledge, and that’s a big step toward protecting your ears and the precious sense of hearing. Here’s to healthy ears and clear hearing for you and your loved ones!