Hearing loss is often seen as a normal part of aging – an inconvenience for those who have it and their loved ones.
But research over the past decade has revealed a deeper concern: untreated hearing loss is linked with an increased risk of cognitive decline, including dementia [1].
In fact, scientists are discovering that caring for your ears might also help protect your mind.
This post explores the science-backed connection between hearing loss and dementia, how interventions like hearing aids may reduce that risk, key findings from the groundbreaking ACHIEVE study, and practical advice on looking after your hearing (and, by extension, your brain).
Key Takeaways
- Research suggests that treating hearing loss supports brain health.
- While there is no definitely link between hearing loss and dementia, current research suggests that early intervention can help maintain brain health.
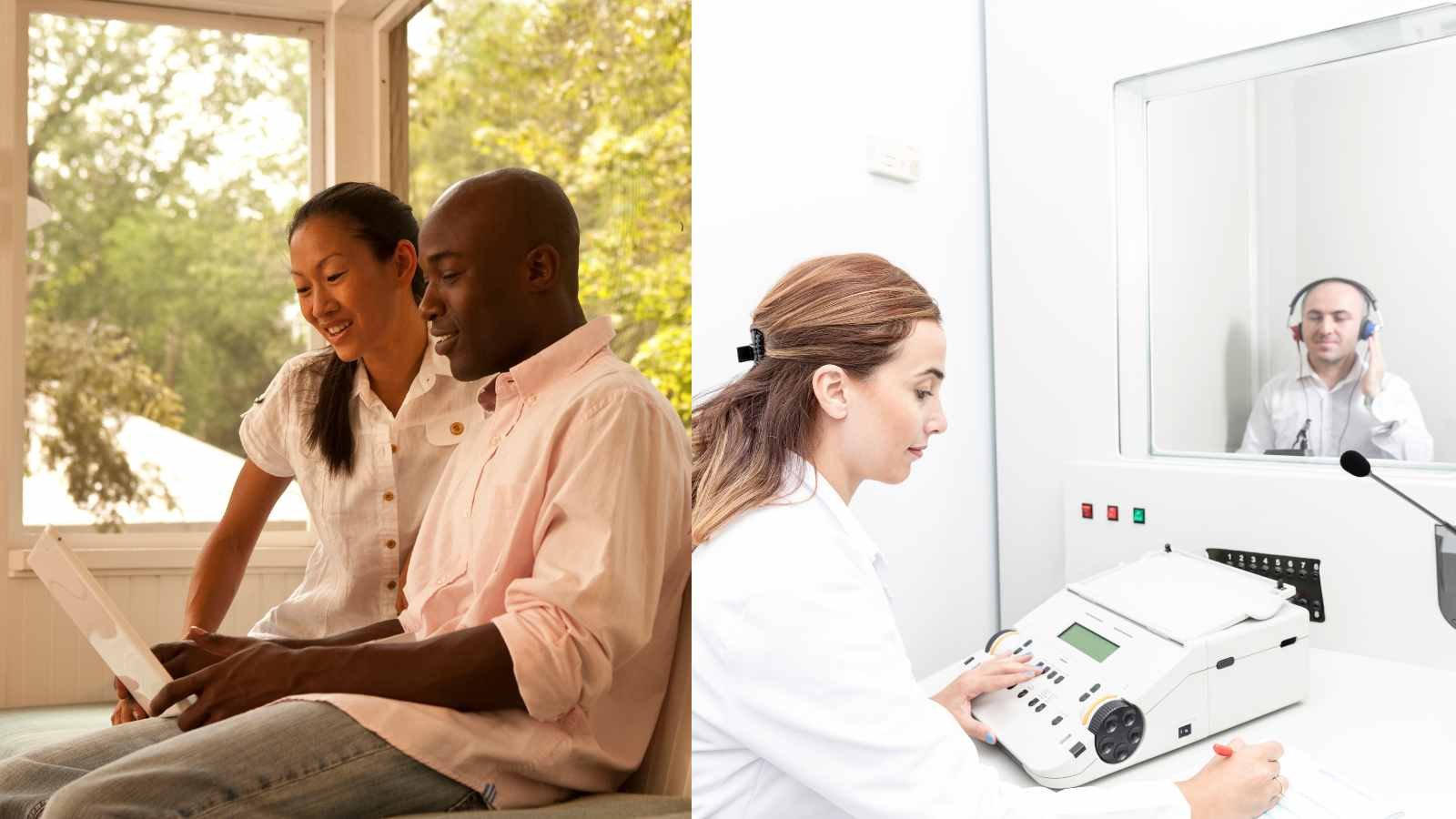
- Establishing a baseline hearing test and rechecking at regular intervals is a good strategy to monitor hearing and intervene at the appropriate time.
How Hearing Loss Affects the Brain and Memory
Hearing loss is extremely common in older adults. Approximately two-thirds of people over age 60 have some degree of hearing loss [2], and for more than one-third of those over 65 the impairment is significant enough to affect daily communication [3].
Beyond the frustration of missed words or muffled sounds, researchers have found that even mild levels of hearing loss are associated with accelerated cognitive decline.
In one Johns Hopkins study tracking 639 adults for 12 years, mild hearing loss doubled the risk of developing dementia among those with increased risk for cognitive decline [4].
Moderate hearing loss tripled the risk, and severe hearing impairment was associated with five times greater risk of dementia, specifically among those with increased risk factors, not a global finding among all of the cohort with hearing loss [5, 6].
These findings have been echoed by other epidemiological studies around the world, leading experts to recognize hearing impairment as a major modifiable risk factor for dementia [7, 8].
In fact, a 2020 Lancet Commission report estimated that hearing loss may be linked to around 8% of dementia cases globally [9] – meaning that addressing hearing problems could potentially prevent or delay roughly 1 in 12 cases of dementia.
Why would losing some hearing be connected to losing memory or thinking skills? Scientists propose several, often overlapping, explanations:
- Brain changes from lack of input: When your ears struggle to pick up sound, the hearing centers of your brain receive less stimulation. Over time, this “use it or lose it” effect may lead to faster atrophy (shrinkage) in parts of the brain [10]. Brain imaging studies show that older adults with hearing loss tend to have accelerated volume loss in key brain regions, which could make them more vulnerable to cognitive decline [11].
- Increased cognitive load: With untreated hearing loss, the brain has to work overtime to decode garbled sounds and speech. This extra effort is thought to come at the expense of other mental processes like memory. As one expert puts it, your brain might be subconsciously “multitasking” just to understand conversations, leaving fewer resources to focus on forming memories or making decisions [12]. Over the long term, this constant strain could contribute to cognitive fatigue.
- Social isolation and depression: Hearing difficulties can cause people to withdraw from social activities because conversations become challenging [13]. You might avoid restaurants, stop chatting on the phone, or feel left out in group settings. Unfortunately, social isolation and loneliness are well-known risk factors for cognitive decline and dementia [14, 15]. If hearing loss leads you to interact less, it can indirectly accelerate memory and thinking problems by reducing the mental stimulation and emotional support that come from engaging with others.
- Common underlying factors: It’s also possible that certain factors (like aging, cardiovascular health issues, or inflammation) independently contribute to both hearing loss and dementia. Researchers work hard to account for these confounding factors in studies. While not all aspects are fully understood, the bottom line is that hearing loss is consistently linked with faster cognitive decline across numerous studies [16, 17]. This doesn’t mean hearing loss inevitably causes dementia; rather, it suggests it can be a significant contributing factor over time.
The good news is that unlike some risk factors for dementia, hearing loss is treatable. We have tools – hearing aids, cochlear implants, auditory training – that can partially restore hearing or help the brain compensate for hearing deficits.
This raises an encouraging question: if untreated hearing loss is bad for the brain, could treating hearing loss be good for the brain?
In other words, can using a hearing aid or other intervention actually reduce the risk of dementia? Researchers have been actively studying this, and the results are promising.
Can Hearing Aids Help Reduce Dementia Risk?
Evidence from multiple studies suggests that older adults who address their hearing loss tend to maintain sharper mental function than those who leave it untreated.
In one large analysis of 31 studies involving over 137,000 people, hearing aid users had a 19% lower risk of cognitive decline over time compared to non-users [18]. They also performed slightly better on tests of memory and thinking (about a 3% improvement on average) than people with hearing loss who did not use any hearing devices [19].
These benefits could stem from an improved ability to engage socially and cognitively – for example, hearing aids help people participate in conversations, which can stave off the disconnection and loneliness linked to dementia [20].
Another compelling piece of evidence comes from observational research on hundreds of thousands of older adults. A 2023 analysis of the UK Biobank cohort (over 437,000 participants) found that people with untreated hearing loss had about a 42% higher risk of dementia compared to those with normal hearing.
In contrast, those with hearing loss who did use hearing aids showed no significant increase in dementia risk – their risk was about the same as people with no hearing loss [21].
In other words, using hearing aids appeared to erase the extra risk associated with hearing impairment.
“Our study provides the best evidence to date to suggest that hearing aids could be a minimally invasive, cost-effective treatment to mitigate the potential impact of hearing loss on dementia,” said Dr. Dongshan Zhu, the lead author of that UK Biobank study [22].
Of course, these kinds of studies have limitations. People who choose to wear hearing aids might differ in other ways from those who don’t (perhaps they’re more health-conscious, or have better access to healthcare), which could partly explain the difference in cognitive outcomes.
To truly demonstrate cause and effect, what’s needed is a randomized controlled trial – an experiment where some people with hearing loss get an intervention (like hearing aids) and others do not, and then their cognitive trajectories are compared.
For a long time, no such trial had been completed. That changed recently with the ACHIEVE study, a major clinical trial led by researchers at Johns Hopkins with support from the National Institute on Aging.
The ACHIEVE Study: Testing Hearing Intervention for Brain Health
The Aging and Cognitive Health Evaluation in Elders (ACHIEVE) study is the first large randomized trial to directly test whether treating hearing loss can slow down cognitive decline in older adults [23].
Beginning in 2018, the trial enrolled 977 adults aged 70 to 84, all with mild-to-moderate hearing loss but no substantial cognitive impairment at the start [24].
The participants were recruited at four U.S. sites and came from two groups: 238 individuals were part of an ongoing heart health study (a group considered at higher risk for cognitive decline due to age and other factors), and the remaining 739 were healthy volunteers from the community [25, 26].
The participants were randomly assigned to one of two groups. One group received a comprehensive hearing intervention – they were fitted with high-quality digital hearing aids (free of charge), received a “hearing toolkit” for self-management, and had regular check-ins with an audiologist for coaching and maintenance [27].
The other group, serving as a control, participated in a structured health education program about aging wellness (covering topics like nutrition, exercise, and chronic disease prevention) but did not receive hearing aids [28, 29]. This way, both groups had regular interactions and support, but only one group got treatment specifically targeting hearing loss.
All participants underwent yearly assessments of their cognitive functions (memory, attention, etc.) over a three-year period [30].
The ACHIEVE trial’s initial results were reported in July 2023 at the Alzheimer’s Association International Conference and published in The Lancet.
The headline finding was nuanced but important: For the overall study population, there was no statistically significant difference in cognitive decline between the hearing intervention group and the control group after 3 years [31].
However, when the researchers zoomed in on the subgroup of participants who had higher risk (those from the heart health study), a striking pattern emerged.
In this higher-risk group, those who received the hearing intervention experienced about 48% less cognitive decline over three years compared to their counterparts in the control group [32, 33].
In other words, their rate of losing memory and thinking abilities was cut nearly in half by actively treating the hearing loss. This is a significant slowing of decline – essentially resembling the difference of almost 3 extra years of healthy brain aging versus the control group.
Why didn’t the hearing treatment show an effect in the healthier subgroup or the overall group? The researchers believe it comes down to the rate of cognitive change.
The community volunteers (the “low-risk” participants) were generally experiencing very slow cognitive decline to begin with – so slow that over just three years, it was hard to detect any difference between those who got hearing aids and those who didn’t [34, 35].
In contrast, the higher-risk subgroup had a much faster rate of cognitive decline (nearly three times faster on average during the study) [36]. This faster decline provided more opportunity for the hearing intervention to make a measurable difference within the study’s timeframe.
Essentially, if your cognition is already slipping noticeably, treating hearing loss might help slow that decline; but if your cognition is initially stable and changing only very gradually, a three-year period may be too short to see an effect from hearing aids.
The ACHIEVE team is continuing to follow all the participants beyond the initial three years to see if differences start to appear in the broader group over a longer period [37].
Notably, the ACHIEVE study confirmed that treating hearing loss is safe and can substantially improve communication and social engagement.
People in the hearing intervention group reported better hearing and communication abilities (no surprise), whereas the control group did not improve on those measures [38]. This reinforces that even if cognitive benefits might take time to become evident, there are immediate quality-of-life benefits to addressing hearing loss.
Researchers and public health leaders are encouraged by ACHIEVE’s findings. “The hearing intervention had a significant effect on reducing cognitive change within three years in the population of older adults at increased risk for cognitive decline,” says Dr. Frank Lin of Johns Hopkins, the co-principal investigator of ACHIEVE [39].
He notes that hearing loss is highly treatable in later life, which makes it an important public health target for reducing risk of cognitive decline and dementia (much like managing other risk factors such as hypertension, social isolation, and physical inactivity) [40].
Likewise, Dr. Maria Carrillo, chief science officer of the Alzheimer’s Association, remarked that hearing loss may be “the single largest dementia risk factor that can be addressed or modified with existing tools that remain underutilized” [41] – underscoring how vital it is to translate this research into action.
In short, while hearing loss is not the sole cause of dementia, it’s one risk factor we can actually do something about. The ACHIEVE trial provides real evidence that doing something about it (like using hearing aids) can make a difference, especially for those most vulnerable to cognitive decline.
Prioritize Hearing Health as Part of Dementia Prevention
What do these findings mean for you or your loved ones? The clear takeaway is that taking care of your hearing is an investment in your long-term cognitive health.
Addressing hearing loss won’t guarantee you never develop dementia, since dementia has many causes, but it could help reduce your risk – and it will certainly improve your ability to stay socially connected and engaged, which itself benefits the brain. On the flip side, ignoring hearing problems can have cumulative negative effects.
Unfortunately, many people wait far too long to seek help for hearing loss. Dr. Lin points out that the average older adult with hearing loss waits 10 years before getting hearing aids, during which time communication with loved ones suffers and social isolation and health risks increase [42]. It’s easy to procrastinate or live in denial about hearing difficulty, but early action can make a huge difference.
Here are some practical steps and compassionate advice for maintaining your hearing health and protecting your mind:
- Get your hearing tested regularly. Don’t assume you’ll “just know” when your hearing declines – many changes are gradual. Annual check-ups often overlook hearing, so be proactive. Experts recommend getting a baseline hearing evaluation by age 50, and then at least every few years thereafter [43]. (more frequently if you notice problems or have risk factors). If you’re over 60 or have a family history of hearing loss, consider making a hearing test part of your routine health screenings. These tests are painless, and they give you an objective measure of your hearing ability. Catching hearing loss early means you can address it before it takes a toll on your cognitive and social well-being.
- Use hearing aids or other assistive devices if recommended. Modern hearing aids are quite advanced – they’re smaller, smarter, and more affordable than those of decades past. If an audiologist determines you have hearing loss, don’t delay treatment. Research shows that properly fitted hearing aids can significantly improve your quality of life and may help preserve cognitive function [44, 45]. There’s essentially no downside to using hearing aids when you need them; they help most people who try them and can “make all the difference in the world” by allowing you to reengage with friends and family [46]. It might take time to adjust to hearing aids, but stick with them – your brain needs consistent auditory stimulation to reap the benefits. If traditional hearing aids aren’t enough (in cases of severe loss), ask about other options like cochlear implants. The key is not to simply live with untreated hearing loss when solutions are available.
- Protect your ears from noise. Prevention matters too. Much age-related hearing loss actually results from a lifetime of noise exposure causing wear and tear on the delicate structures of the inner ear. You can reduce further damage by avoiding excessively loud environments or using ear protection (earplugs or noise-cancelling earmuffs) when you can’t avoid the noise. This is especially important if you’re mid-life – protecting your hearing in your 40s, 50s, and 60s could mean you have better hearing (and possibly a lower dementia risk) in your 70s and beyond. Even simple steps like turning down the volume on music and being cautious with headphones can help preserve your hearing longer. Your ears and brain will thank you later.
- Stay socially engaged and mentally active. Treating hearing loss goes hand-in-hand with staying connected. Make the effort to maintain your social ties, pursue hobbies, and engage in conversation – even if it requires some accommodations like using assistive listening devices or choosing quieter venues. Social interaction and mental stimulation are known to support brain health. If you’ve gotten hearing aids, use them consistently to help you participate fully in life. And don’t be shy about telling friends and family what you need (like speaking clearly or facing you when talking). Keeping communication flowing not only improves relationships, it gives your brain a healthy workout. Hearing well is part of that, but so is the confidence and willingness to keep interacting despite any hearing challenges.
Finally, if you or someone you care about is experiencing hearing difficulties, approach the issue with compassion – both for yourself and others.
There can be stigma and emotional hurdles around admitting hearing loss or wearing hearing aids. Remind yourself and your loved ones that caring for your hearing is an act of self-care, not an admission of defeat. Just as we treat our eyes with glasses or our blood pressure with medication, treating hearing loss is simply a way to take care of our health.
And now we know it might also protect our minds from decline. “Until we know more,” Dr. Lin advises, “we recommend for general health and well-being that older adults have their hearing checked regularly and any hearing issues properly addressed” [47].
In the end, preserving your hearing and your cognitive health is about maintaining your independence, relationships, and quality of life.
Conclusion
The link between hearing loss and dementia is real, but it comes with a hopeful message. By catching hearing loss early and treating it – whether through hearing aids, implants, or other strategies – we may give ourselves a better chance at staying mentally sharp in our later years.
Hearing loss doesn’t just affect the ears; it affects the whole person. So if you’re entering your senior years (or caring for someone who is), remember that a hearing test could be just as important as a memory test. Protect your ears, stay connected, and don’t hesitate to seek help for hearing problems.
Taking action on hearing health is a gentle, practical step that can make a meaningful difference in the journey of healthy aging [48]. Your hearing matters, and so does your brain – and tending to one may well benefit the other.